Home » News and events »
First patient treated in cutting-edge rare liver disease clinical trial

Research theme
People involved
Associate Professor and Honorary Consultant Hepatologist
The first patient has been recruited to the FARGO clinical trial, which is testing a new treatment to improve quality of life for patients living with primary sclerosing cholangitis (PSC), a rare liver disease.
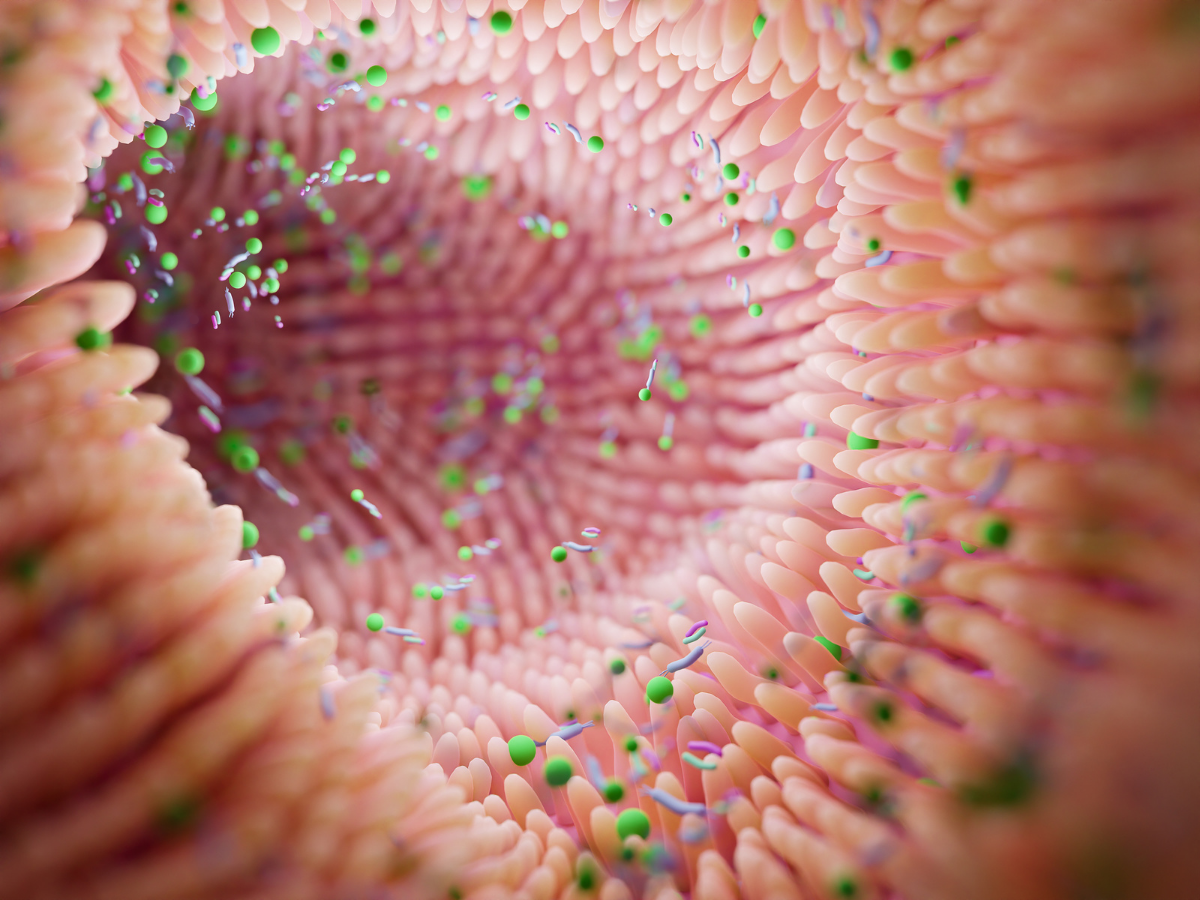
The trial, funded by the not-for-profit medical research charity Lifearc and PSC Support and run by the University of Birmingham with the support of the National Institute for Health and Care Research (NIHR) Birmingham Biomedical Research Centre, will investigate the potential of faecal microbiota transplantation (FMT) to correct the imbalance of the gut microbiome in people with PSC, with the hope that this could slow or even reverse progression of the disease.
FARGO is the first ever multi-centre double-blind placebo-controlled trial of FMT in PSC, and it aims to recruit 58 patients across Birmingham and further participating sites in England including the Royal Free London, St Mark’s Hospital, Imperial College London, and Norfolk and Norwich University Hospitals NHS Foundation Trust.
People taking part in the study will receive either FMT once a week for eight weeks, or placebo. The FMT procedure involves collecting stool from healthy donors and refining it in a laboratory before transferring it to the bowel of people with PSC. The first administration is done via the annual routine colonoscopy undertaken by PSC patients, to optimise patient experience and avoid unnecessary additional appointments; additional courses of FMT are then administrated via enema for the following seven weeks.
Previous research has shown that FMT is safe and effective in treating inflammatory bowel disease and Clostridioides difficile infection. The trial builds on the expertise and support of the University of Birmingham’s Microbiome Treatment Centre (MTC), the first Medicines and Healthcare products Regulatory Agency (MHRA) licensed facility in the UK to provide FMT for clinical trials and for the treatment of patients with recurrent and refractory Clostridiodes difficile infection.
The trial will be run at the Birmingham Cancer Research UK Clinical Trials Unit (CRCTU), which is globally renowned for its academic excellence and enables innovative research with the potential to change lives, in both cancer and non-cancer fields like inflammatory diseases.
“….this is the first time worldwide that FMT treatment is being investigated for patients with the disease.”
Dr Palak Trivedi, FARGO trial lead
Trial lead Dr Palak Trivedi, Clinician Scientist at the NIHR Birmingham Biomedical Research Centre, Associate Professor at the University of Birmingham and Consultant Hepatologist, said:
“We are very excited to have our first patient joining this innovative trial. There is currently no cure or medication for primary sclerosing cholangitis, and this is the first time worldwide that FMT treatment is being investigated for patients with the disease.
“We are grateful to our patients for helping us in our mission to find new treatments that may significantly improve the lives of people affected by this devastating disease.”
New hope for patients
Rick Dallaway is the first patient to take part in FARGO after first being diagnosed with PSC and IBD in January 2016 following months of weight loss, fatigue, night sweats and brain fog.
Dallaway, who is also a trustee of the charity, PSC Support, lives in Birmingham and works with specialist PSC doctors based at University Hospitals Birmingham NHS Trust, where they treat both conditions together.
Rick reflected on finding out he had Primary Sclerosing Cholangitis and IBD: “The diagnosis came only a matter of weeks since visiting my GP. I was lucky that I received a diagnosis quickly because I have since learned that some patients have to wait a long time to get an accurate diagnosis of PSC usually because they are unable to be seen by a hospital with the specialist staff.
“…it is worth [taking part in the trial] to further our understanding of this disease and I strongly believe there will be some good data coming out of this trial to benefit everyone in the PSC community.”
Rick Dallaway, first participant in the FARGO trial
“At the time it felt like a ‘double whammy’ being diagnosed with two conditions at the same time – PSC and IBD. it felt like my IBD was the more serious of the two because I was having unpleasant symptoms and I was pleased that I was given medication to bring this under control. I found the charity PSC Support which introduced me to a community of great people, and provided me with up-to-date and accurate information about the condition. Since my diagnosis with PSC, I have continued to suffer from fatigue, brain fog and some mild itching.”
Through appointments with the clinic at the Queen Elizabeth Hospital, Rick heard about and was able to sign up to the FARGO trial as patient number one.
Rick continued:
“The trial resonated with me as I have an interest in the microbiome and its effect on wellbeing, so it seemed the perfect trial for me. The trial requires enemas and colonoscopy so it isn’t as easy as taking a tablet, but it is worth it to further our understanding of this disease and I strongly believe there will be some good data coming out of this trial to benefit everyone in the PSC community.
“I am patient number one on the trial and have just completed the most demanding part of the trial which requires an initial assessment followed by 8 weekly visits, all of which require a treatment of FMT (or placebo). Next, I will have appointments every 3 months or so until the trial ends 48 weeks after my initial screening.
“My experience of the trial is extremely positive. The trial nurses at Birmingham are helpful, very accommodating in arranging the weekly appointments, and have put me at ease at every step of the journey. I am really looking forward to the results coming out for the trial.”
Dr Catriona Crombie, Head of Rare Disease at LifeArc, adds: “Should this trial show that FMT works well, PSC Support will be advocating for patients to access FMT as early as possible. We hope this means it will be making a difference to patients within five years after we’ve completed this work.”
-
Notes to editors
- For media enquiries please contact Tim Mayo, Press Office, University of Birmingham, tel: +44 (0)7815 6070157
- The University of Birmingham is ranked amongst the world’s top 100 institutions. Its work brings people from across the world to Birmingham, including researchers, teachers and more than 8,000 international students from over 150 countries.
- The University of Birmingham is a founding member of Birmingham Health Partners (BHP), a strategic alliance which transcends organisational boundaries to rapidly translate healthcare research findings into new diagnostics, drugs and devices for patients. Birmingham Health Partners is a strategic alliance between seven organisations who collaborate to bring healthcare innovations through to clinical application:
- University of Birmingham
- University Hospitals Birmingham NHS Foundation Trust
- Birmingham Women’s and Children’s Hospitals NHS Foundation Trust
- Aston University
- The Royal Orthopaedic Hospital NHS Foundation Trust
- Sandwell and West Birmingham Hospitals NHS Trust
- West Midlands Academic Health Science Network
- Birmingham and Solihull Mental Health NHS Foundation Trust
- Primary sclerosing cholangitis (PSC) is a rare liver disease where the body attacks itself, causing inflammation and scarring of the bile ducts and liver. This causes bile to stop flowing properly, leading to repeated infections, liver failure and, in some cases, cancer. In 80% of people with PSC the body will also attack the bowel, which can lead to inflammatory bowel disease (IBD).
There is still no cure for PSC, and liver transplantation is the only lifesaving treatment for some PSC patients. It is, however, risky and costly to the NHS, and PSC returns in around a third of people who have had a liver transplant.
This experimental FMT treatment builds on previous evidence suggesting that the gut microbiome is involved in the way PSC develops and progresses. Research has shown that the microbes present in the gut of people with PSC are different to those in people without liver and bowel inflammation – and this gut microbe imbalance is linked with many abnormal immune functions, which may drive development of the condition.
Patients must be UK residents to enrol in the FARGO trial.
- LifeArc is a self-funded, not-for-profit medical research organisation and charity. We take science ideas out of the lab and help turn them into medical breakthroughs that can be life-changing for patients. We have been doing this for more than 25 years and our work has resulted in five licensed medicines, including cancer drug pembrolizumab (Keytruda®), lecanemab for Alzheimer’s (Leqembi), and a diagnostic for antibiotic resistance. Our teams are experts in drug and diagnostics discovery, technology transfer, and intellectual property. Our work is in translational science – bridging the gap between academic research and clinical development, providing funding, research and expert knowledge, all with a clear and unwavering commitment to having a positive impact on patient lives.
LifeArc is a company limited by guarantee (registered in England and Wales under no. 2698321) and a charity (registered in England and Wales under no. 1015243 and in Scotland under no. SC037861).
Find out more about our work at the LifeArc website.